By: Prof. Dr. Seyed Saeid Zamanieh Shahri, MD and Prof. Dr. Sonia Sayyedalhosseini, MD
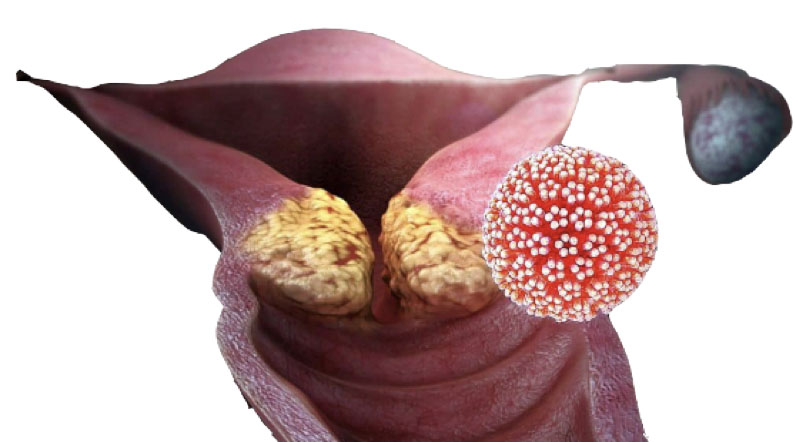
Cervical cancer is a type of cancer that occurs in the cells of the lower part of the uterus and vagina. Cervical cancer occurs when cervical cells grow abnormally and multiply rapidly. For example, one of the factors that cause cervical cancer is contact with the human papilloma virus, which causes mutations in cervical cells. This mutation causes normal cells to become abnormal cells. Abnormal cells accumulate and form a mass called a tumor. A mass or tumor in the cervix can be benign or malignant. Benign masses of polyps, cysts and warts in the genital area are usually not dangerous and do not invade other surrounding tissues, but malignant masses of cervical cancer are sometimes life-threatening and can invade surrounding tissues and organs or spread to other parts of the body.
Anatomy and physiology of Cervix:
Cervix is the lowest part of the uterus that protrudes into the vagina and creates a space called the fornix. The upper part of the cervix (supra vaginalis) is located above the junction between the vagina and the cervix. The lateral part of the supra vaginalis cervix is connected to the cardinal ligament. Cervix is about 2 to 4 cm long. It contains many secretory glands that secrete mucus.
Causes and Risk Factors:
Infection with HPV, human papilloma virus causes this disease in 90% of cases in women. A person may be infected with this virus for several years and not know about it. When this virus is in a person’s body for a long time, it may show itself gradually and turn some cervical cells into dangerous cancer cells. Of course, in many people, infection with this virus does not cause illness.
The following individuals are also very prone to cervical cancer:
Addicted to smoking.
Taken oral contraceptive pills for 5 years or more.
Had multiple pregnancies and deliveries.
Spouse has multiple sexual partners.
Weak immune system
Have multiple sexual partners.
Started having sex at a young age.
Deficient in vitamin E, C and folic acid.
Obese.
Have no delivery.
Signs and Symptoms:
The most common initial manifestation is abnormal bleeding (after intercourse, between periods, or after menopause).
Abnormal vaginal discharge (may be watery, bloody, mucoid, purulent, or foul-smelling)
The usual presentation is intermittent painless metrorrhagia or spotting that occurs after intercourse.
As the cancer grows, the bleeding episodes become more severe, more frequent, and longer.
Late symptoms of cervical cancer include:
Recurring pain in the side or lower limbs, heartburn, presence of blood in the urine, bleeding from the rectum, irreversible constipation, persistent edema of one or both lower limbs, heavy bleeding and hemolysis, necrosis.
Inflammation and bleeding may cause false positive results in Pap smear.
Stages of cervical cancer:
Stage zero: carcinoma in situ
Stage 1: Limited to the cervix
Stage 2: It has spread beyond the cervix, but has not reached the side walls of the pelvis or the lower third of the vagina.
Stage 3: It has affected the side walls of the pelvis or the lower third of the vagina.
Stage 4: Metastatic disease
Diagnosis:
Annual cervical cancer screening cytology test should be started at the beginning of vaginal intercourse or at the age of 21. In low-risk women, if consecutive tests are normal, the screening test can be performed every three years. In women at higher risk, screening at shorter intervals is recommended. Screening may not be necessary in women older than 70 years who have had at least three consecutive normal tests in the past 10 years or women who have had a total hysterectomy.
Cytology screening tests that are abnormal should be followed up with colposcopy with direct biopsy. All palpable lesions or those that can be seen with the naked eye should be sampled.
In cases where there is suspicion of microscopic invasion or cervical cancer in the early stages, cervical cone biopsy is indicated. This is done to assess the possibility of invasion.
Unlike other genital cancers that are staged through surgery, in this cancer, staging is mostly done through clinical evaluation.
Staging should include observation, palpation, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, venous pyelography, and examination of the lungs and skeleton with X-ray imaging.
Cone biopsy is considered part of clinical staging. Clinical examination may be performed under anesthesia. CT scan and MRI are valuable in treatment planning, but are not used in staging. These methods are useful for checking the condition of the lymph nodes and the spread of the tumor in the pelvis. Laboratory tests include: CBC, BUN and creatinine and liver function tests. These tests evaluate anemia and metastasis. In patients diagnosed with HPV, consider other (STDs) Sexually Transmitted Diseases, especially HIV.
Cervical cancer screening:
Pap smears for all women who are sexually active or who have reached the age of 18. In low-risk women (those with three consecutive normal Pap smears and no history of abnormal Pap smears), Pap smears can be performed every 2-3 years.
Pap smear should be stopped if entire uterus removed due to benign issues. Some groups recommend that smears are not necessary after the age of 56-70 in low-risk individuals whose pap smears have been consecutively normal, but some recommend doing it every 2-3 years. It is variable according to each individual’s disease, family history of cancer, past medical history of cancer or STDs, and etc. So, consult with your doctor about it.
Vaccination against HPV is effective in preventing permanent infection as well as cell abnormalities caused by HPV type 16. Vaccination is likely to change screening guidelines in the future.