By: Prof. Dr. Seyed Saeid Zamanieh Shahri, MD and Prof. Dr. Sonia Sayyedalhosseini, MD
3. Sympathetic nervous system activity:
Increased sympathetic tone can sustain higher blood pressure through elevated vasomotor tone, increased heart rate, and altered baroreceptor sensitivity.
4. Endothelial dysfunction:
Reduced nitric oxide bioavailability and upregulation of vasoconstrictive mediators like endothelin disrupt the balance between vasodilation and vasoconstriction, favoring the latter.
5. Vascular remodeling:
Structural changes such as smooth-muscle hypertrophy, increased collagen deposition, fibrosis of the medial layer, and intimal thickening reduce vascular compliance and raise baseline resistance.
6. Renal mechanisms:
The kidneys regulate extracellular fluid volume, sodium excretion, and tubuloglomerular feedback. Persistent disturbances in these mechanisms can shift the pressure set point upward.
Polygenic genetic effects, developmental programming (e.g., low birth weight), inflammatory pathways, and oxidative stress modulate these physiological systems in an additive manner.
Causes of Hypertension: Hypertension is classified etiologically into two broad categories:
a) Primary/Essential Hypertension: The most common form, with no single identifiable cause. It arises from interactions among genetic predisposition, environmental factors (such as high salt intake, low physical activity, chronic stress), age-related vascular changes, and neurohormonal networks.
b) Secondary Hypertension: Hypertension caused by an identifiable underlying disorder. Examples include:
• Renal parenchymal disease (impaired sodium excretion, reduced nephron number)
• Renal artery stenosis (RAAS activation due to kidney ischemia)
• Endocrine disorders (primary hyperaldosteronism, pheochromocytoma, Cushing’s syndrome, thyroid/parathyroid abnormalities)
• Sleep disorders (obstructive sleep apnea)
• Aortic diseases
• Drug- or substance-induced hypertension (e.g., glucocorticoids, stimulants)
In secondary hypertension, trends in blood pressure often parallel the course of the underlying disorder and may improve once the cause is corrected.
Risk Factors: Risk factors span individual characteristics, genetic susceptibility, biological factors, and environmental influences:
• Age: Arterial stiffness and pressure-enhancing pathways increase with age, raising hypertension prevalence.
• Genetic predisposition and family history: Polygenic contributions involving sodium regulation, vascular tone, and hormone pathways are documented.
• Metabolic and anthropometric factors:
o Visceral obesity
o Insulin resistance
o Type 2 diabetes
o Dyslipidemia
o Low-grade inflammation and oxidative stress associated with these conditions contribute to vascular tone changes and structural remodeling.
• Behavioral/environmental factors:
High sodium intake, alcohol consumption, irregular sleep patterns, air pollution, and chronic stress may elevate baseline cardiovascular pressure.
• Comorbid conditions:
chronic kidney disease, endocrine disorders, and sleep apnea are well-established contributors.
• Ethnic/biological variations:
Epidemiological differences reflect interactions among genetic, epigenetic, and environmental elements.
Signs and Symptoms: Hypertension often remains asymptomatic, facilitating delayed detection. However, some individuals experience nonspecific manifestations such as:
• Episodic headaches (sometimes occipital)
• Sensation of heaviness in the head or dizziness
• Tinnitus or palpitations
• Fatigue
• Blurred vision or visual flickers
• Epistaxis
In more severe forms, especially when pressures rise rapidly, neurologic (altered consciousness or vision), cardiopulmonary (respiratory distress), or renal manifestations may appear.
Distinguishing “chronically elevated blood pressure” from “hypertensive crises” depends on numerical levels, rate of change, and evidence of target-organ injury. Many of these signs also occur in other conditions; therefore, they are not diagnostic on their own.
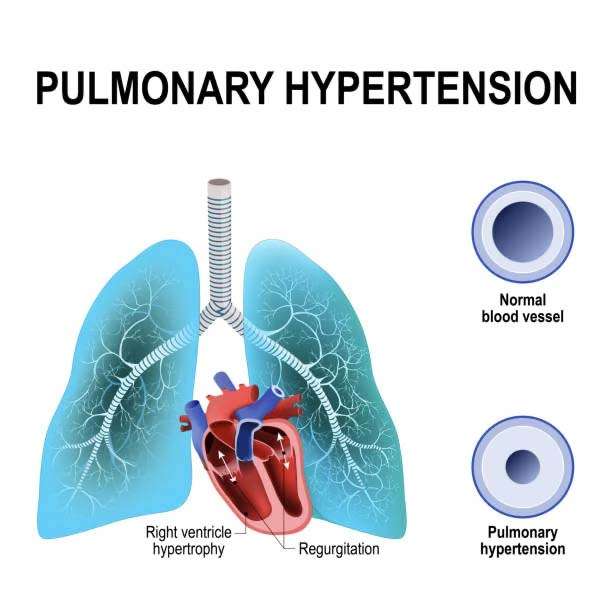
Complication: Chronic elevation of blood pressure produces cumulative and progressive damage across multiple organ systems:
• Heart: Left ventricular hypertrophy (as a compensatory response to chronic afterload), myocardial stiffness, diastolic dysfunction, and in advanced stages systolic dysfunction.
Increased risk of coronary artery disease, heart failure, arrhythmias, and ischemic events.
• Large and peripheral arteries: Accelerated atherosclerosis, aortic stiffening, aneurysm formation, or dissection in some settings. Peripheral vascular involvement can lead to reduced limb perfusion and functional impairment.
• Brain: Increased risk of ischemic and hemorrhagic stroke, transient ischemic attacks, and vascular dementia.
Microvascular brain changes (lacunes, microbleeds, white-matter alterations) correlate with chronic hypertension.
• Kidneys: Hypertension may be both a cause and a consequence of kidney disease.
• Eyes: Hypertensive retinopathy manifests as arteriolar narrowing, flame-shaped hemorrhages, exudates, and optic disc edema, reflecting severity and chronicity.
• Acute consequences: Hypertensive crises can result in acute target-organ damage such as pulmonary edema, hypertensive encephalopathy, acute kidney injury, or intracranial hemorrhage. Overall, the intensity and duration of exposure to elevated pressure correlate with the onset and severity of complications. Reduced vascular compliance and maladaptive renal–neural–hormonal feedback reinforces this cycle.
To be continued …